Infertility journey in IVF Laboratory
There is so much care of your eggs, sperm and embryos that takes place in the IVF laboratory. Each day of the process has specific goals and tasks that are performed.
24 seconds of embryo development in IVF Lab that may change people’s lives…
So what’s in the video above?
With the development of new technology including embryo monitoring systems, embryologists now have a window to see the developing embryo without disturbing the sensitive culture environment. The attached video above shows the development of the embryo from the single cell stage to the expanded blastocyst stage. The embryo can be seen cleaving first to the two cell stage, multiplying to the four and 8 cell stage and then forming the later phased morula. After the morula stage, blastulation occurs and the embryo develops into a fully expanded blastocyst ready for transfer or cryopreservation. Scientists are still analysing this data to determine what information from the hours of footage may be clinically significant and that the information will help predict the implantation potential of the embryos.
Bear in mind that 24 seconds in the video means 5 days of embryo culture and many people involved in the process. So let’s have a look how it really works in an IVF Lab and what’s the role of the embryologist in the IVF treatment process… Let’s start from the beginning.
The infertility journey can often begin with learning a new language. ICSI, AZH, PGS IVF, IUI and other abbreviations can feel overwhelming! I see many couples try to gain some control of their process and navigate their journey with a complicated and sometimes idiopathic diagnosis.
Often there are other infertility treatments started in the clinical setting before IVF is even recommended. As a couple struggling to become pregnant, it can feel like the process takes forever; waiting on appointments, blood work, and treatment plans. However once the letters “IVF” are uttered from a clinician, the treatment process accelerates including testing, medication administration and clinical monitoring.
Many patients do not know what an important role the embryology lab plays during their treatment process. Not only is there not much information on the IVF Laboratory, but the field of embryology itself is not widely talked about.
Embryology laboratory and quality
An embryology laboratory is typically directed by an individual with strict qualifications including a PhD or MD. The Laboratory director works very closely with the clinicians and medical directors to provide you with quality care using embryologists and laboratory professionals. Each state regulates the licensing requirements of laboratory professionals and these qualifications are reviewed by accreditation agencies.
An embryology laboratory is designed to provide a specialized cell culture environment. The whole lab is designed to mimic the fallopian tube and uterine environment. The air quality, environment, materials and safety protocols that are used are very specialized.
Air quality is a very important component of a successful IVF/Embryology Laboratory. Many labs have a designated ventilation system with HEPA filters and carbon filters to ensure only the cleanest air possible is inside the laboratory. City pollution, cleaning products, laminate countertops and carpet shampoo are all examples of potentially toxic sources that inhibit embryo development. In my laboratory we use a designated ventilation system for the lab and surrounding oocyte retrieval and embryo transfer suites. It has 4 separate filter systems and the maximum number of fresh air exchanges. Our owner and clinician even chose our location based on wind patterns that ensured less polluted air from Northern Minnesota instead of air from the more highly trafficked, highly populated inner-city areas.
You Might Be Interested In
- How to Prepare for IVF Embryo Transfer, Before and Afterwards
- What to Do and What Not to Do After Embryo Transfer?
- Donor Egg IVF Success Rates – The Truth Clinics Don’t Tell You
The environment in an IVF Lab
The environment of the IVF/Embryology Laboratory is also tightly controlled. Research has shown that embryos may be sensitive to light, as no light reaches them as they grow inside the body, therefore the laboratory likely has little or no natural light, is warm and very humid. The embryos must be transported around the lab during various procedures, so we keep the temperature warm to prevent rapid cooling of the dishes they are carried in, and keep all of the equipment and working surfaces at 37 C. We also control the humidity if possible to prevent evaporation of our media, which would cause a change in osmolarity and affect the embryos access to various proteins and sugars needed to grow. Embryologists often wear scrubs, hair covers, gloves and masks to protect ourselves from biologicals and to prevent contamination of the culture systems. There is a very fine balance between aseptic culture and nurturative culture. Over using cleaning products in attempt to be as aseptic as possible can create toxic air and the wrong type of gloves can be detrimental. Construction materials in the design and building of the lab can impact cell growth as well, and off gassing of laminate, flooring and cabinets can affect air quality. A lab that tests and considers all possible sources of air contamination will have higher success.
Embryo culture
Embryo culture and gamete processing requires the use of consumable products such as collection containers, culture dishes and centrifuge tubes that are usually manufactured using plastics. Many labs use a bioassay to test these materials and to verify they do not have an effect on cell culture. Labs also have the option of buying materials that have been pre-tested and proven safe. Each lot (or box) must be verified to make sure no variation in product manufacturing is detected. This way, we can trust that any variation in cell behaviour is due to the cell itself, not because of the container it is living in. For example, we are very particular about those semen collection containers. It is why we provide collection kits and the home Tupperware, film case or prescription bottle are not usable. If your sample is determined to be below the normal parameters, we want to make sure the container it was collected in did not impact the test results.
The media we use to grow and nurture your gametes is also strictly regulated. It is often formulated from synthetic human fallopian tubal fluid. The substrates in the media provide energy to oocytes, sperm and embryos so they can grow and develop. Most types of media need warming and equilibrations before use. We prepare your dishes and tubes the day before to ensure it is optimized for the cell type. The environment the cells are cultured in is different than room air and temperature. This means we need to strictly control culture conditions to make sure that it is as close to what the average uterus/fallopian tube is like. CO2, O2 and temperature are measured every day to make sure systems are safe and optimal. We spend a significant amount of time dedicated to quality control and documentation each day.
After the embryologists make sure the environment and materials are safe, the work begins. We begin early in the morning, perform quality control measures and begin to prepare for the day. When looking at a clinic’s website you want to make sure the lab is accredited and that the clinic has appropriate staffing. Degree requirements and staffing ratios are listed in “Revised minimum standards for practices offering assisted reproductive technologies”1 by the CDC.
IVF Laboratory Preparation
We prepare for your gametes in the lab first administratively. We receive information and orders from your clinician about the different types of laboratory treatment your gametes will be receiving. We need to know if you are using your own eggs or sperm (or using donor eggs or sperm), coordinating where and when the specimens will be available and what fertilization, culture, transfer, biopsy and freezing options the clinician has ordered for you. The day before your retrieval procedure we begin by preparing and filling your dishes and tubes. Day 0 or retrieval day is the day our work with the oocytes begins!
Embryo development in IVF Lab – 5 days that may change people’s lives
Egg retrieval day – Day 0
We are involved in your egg retrieval by looking for and identifying eggs from aspirated follicular fluid. After the egg retrieval procedure, the eggs rest. Depending on the method your clinician chooses for fertilization, the eggs will be treated to remove their cumulus cells for ICSI or washed and placed in droplets for conventional insemination.
If ICSI is selected and the cumulus cells are removed and the eggs will begin a process where a tiny little needle is used to pick up and inject the best morphologically shaped, motile sperm into the cytoplasm of your eggs. Morphology is the term used to assess or describe the shape of the sperm head. The more normal/oval the sperm head shape is the higher the chance that the nuclear material inside the sperm head is normal too.
I always love a “it’s all about the looks” joke here when I talk to patients.
Sperm motility is used to assess viability and is an indicator that the sperm is alive and capable of fertilizing an egg. If a patient has no motile sperm, viability may still be identifiable, but your prognosis is reduced. The typical normal fertilization rate or success with ICSI is 75%. An important reminder for patients……not all eggs are equal.
During this ICSI process egg morphology is also evaluated and noted. While we can’t see the nuclear or DNA material of the egg, other morphological factors like granularity and refractile bodies may be noted in some or all eggs and communicated to the clinicians. Embryologists may have insights based on these first evaluations of your gametes that may help the clinician alter a treatment plan. While we have learned a lot about egg and sperm quality and development, there is still much we don’t yet know. The way that the egg and sperm look may be an indicator of its quality, or potential for success, however there are gametes on both sides of the morphology spectrum that can create beautiful babies.
We attempt to fertilize everything with the best gametes we have and go from there.
Something I have shared many times over the years that has seemed to connect with patients is the grocery store analogy. When a person goes to the grocery store and opens a carton of eggs, they look very similar and good. This is not the case in a human dozen.
Even in optimal donor egg cases, I see variability. This makes sense if you consider that all of the follicles that the eggs were aspirated received the same dosage of medication in your bloodstream. Even the follicles responded differently from this medication. Some measured 13mm and some 21mm. The reason some follicles, eggs etc responded appropriately and inappropriately can give us some insight that some eggs were never meant to be ovulated or create a pregnancy. Embryology still isn’t reparative, only nutritive of what you already have. 20 eggs will not likely translate into 20 embryo, blastocysts or infants, even with a fertile egg donor.
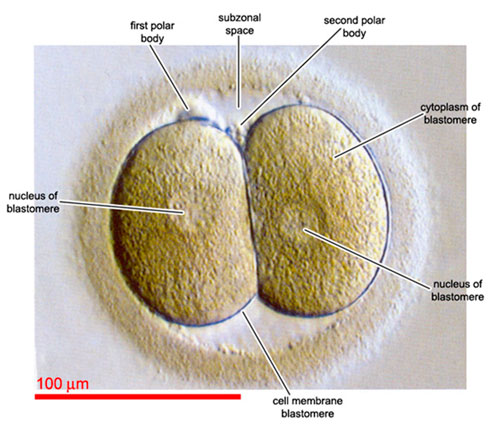
Each lab has a defined optimal window for this evaluation and it usually occurs the morning after your retrieval. The embryologist is looking at the embryos with a high-powered microscope to see if normal fertilization occurred. This can be determined by making sure we see 2 pronuclei in your embryos. One pronuclei is the maternal contribution to the embryo and the second pronuclei is the paternal component (the other copy is expelled from the cytoplasm in the form of a polar body). Embryos that exhibit abnormal fertilization are discarded and usually only the embryos that exhibit normal fertilization are placed in culture dishes with fresh media that have everything they need to grow and placed back in the incubators for the rest of the day and night after evaluation.

Abnormal fertilization:

Embryo growth evaluations – Day 2 to Day 4
Each lab has their own systems based on the media and equipment that are used that determine how often and when evaluations are made. Some labs change media every 48 hours and evaluate daily while some labs culture through with no evaluations until day 5. Other factors that may impact the number and when evaluations are performed are the number of embryos, day of embryo transfer and whether your clinic performs fresh or frozen transfers.
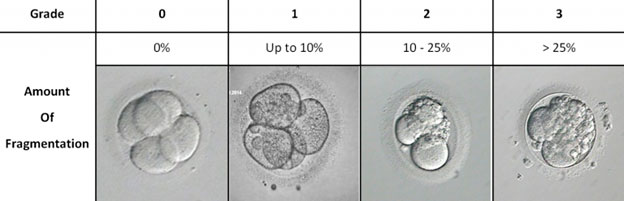
Growth evaluations can provide two functions. They can be used to change media (and nutrients) and to evaluate the beginning stages of development in the lab. Embryos on day 2 ideally range from 2 to 4 cells and have a low degree of fragmentation, balanced cell symmetry and an overall quality designation. Fragmentation is the blebbing of extracellular material from the blastometers, the cells that makeup the embryo at this stage.
No one is 100% sure what causes an embryo to fragment, but it is a prognostic indicator. That means that embryos that have a high degree of fragmentation have a reduced chance of implantation.2
That doesn’t mean if an embryo is fragmented it won’t implant and result in a healthy pregnancy and fetus or that if you transfer an embryo with a low degree of fragmentation that it will always result in success. The function of the fragmentation evaluation is for information about the treatment cycle, laboratory quality control and how the patient’s cells are responding the laboratory environment.
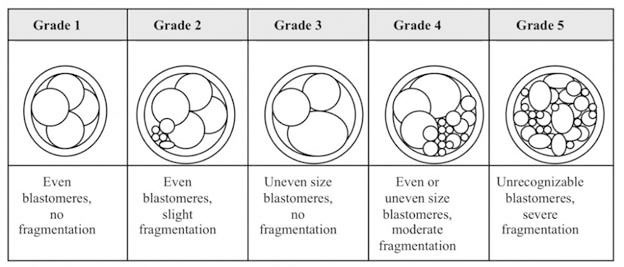
Embryologists also evaluate cell symmetry during their growth assessment. Symmetry is an indicator that each cell group is dividing. For example, if you have a three-cell asymmetrical embryo, maybe one of the two cells cleaved, but the second did not and appears as one big cell. An asymmetrical embryo also has a reduced prognosis. The overall embryo quality of an embryo has been standardized by the Society of Assisted Reproductive Technology (SART.org).[3,4,5]
Embryo fragmentation grading:
Embryo grading:
A typical look of embryos in the microscope looks like this:
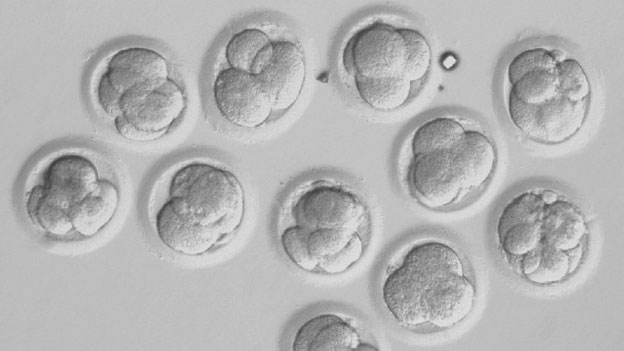
As you can see above – there are many different embryos in different stages with different degrees of fragmentation, symmetry and quality. Embryologists use those parameters to select the embryos with the best prognosis for pregnancy.
You may be also interested in reading:
The Good, The Bad And The Baby Maker – Embryo Quality – Grading Systems
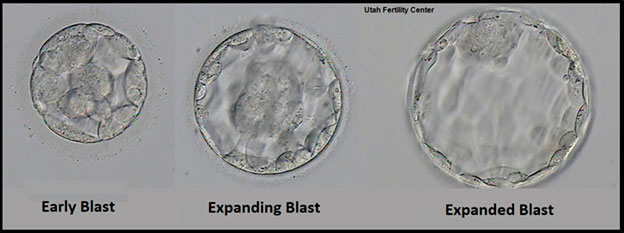
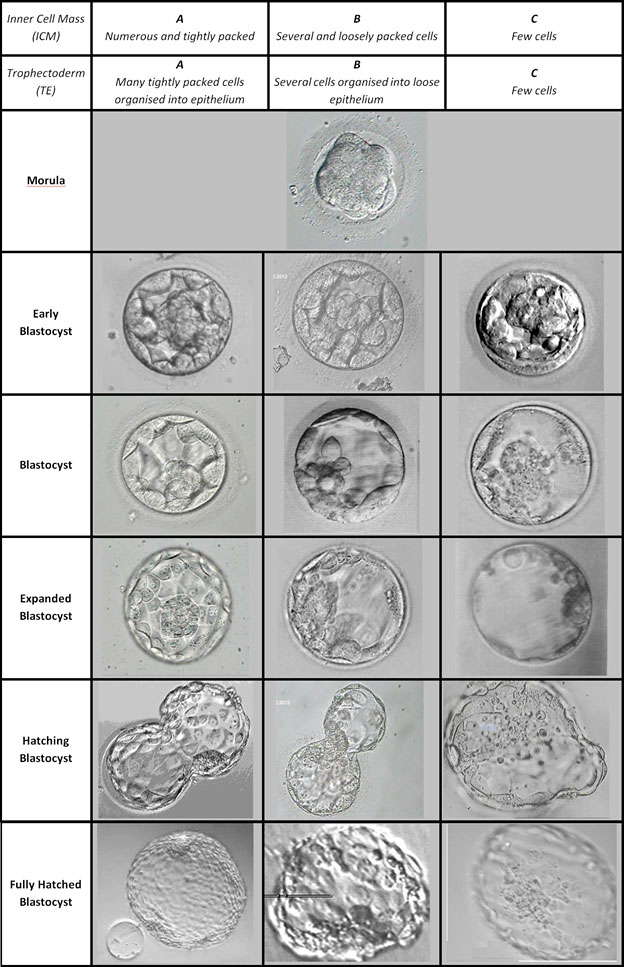
Preparation for the embryo transfer – Day 5 (but also applicable for Day 2 or Day 3 transfers)
On the day of your scheduled embryo transfer the embryologist is going to evaluate all of your embryos. They are evaluating all of your embryos individually for attributes that have been proven to be linked to higher implantation potential. These attributes are different for different stages of development.
We pick the best you have. Every person’s embryos are different.
If you have more embryos than your clinician has approved to transfer that have these positive attributes, we may recommend that you cryopreserve any supernumerary embryos. Expectations can be very challenging during this time…
A fully expanded or hatching blastocyst with a tightly packed inner cell mass and organized trophectoderm is a desired embryo for transfer. But whether a blastocyst is in the early stages or hatching can also depend on the timing of retrieval and transfer. So, the embryologist will select the best embryo available to transfer and anxiously await your pregnancy tests too! Having extra embryos to freeze or high-quality embryos to transfer does not guarantee success and conversely having no embryos to freeze or poor quality embryos do not mean failure so it is important to try to keep an open mind and wait until your final test results for next steps and plans for the future.
Each gamete/embryo is in a different phase of care on any given day. Some patients are having eggs and sperm retrieved and some patients are having embryos transferred and there are culture stages everywhere in between. Scheduling, communication and systems to facilitate the preparation and treatment of the varied patients are critical.
Most of what embryologists do are dependent on schedules and timing. Many protocols have optimal intervals and we can’t go home when the clock chimes. We go home when the work is done and everything is ready for the next day.
Because what we do requires preparation, an unscheduled change can be disruptive to the flow. It is helpful for you to be on time for your appointment, follow instructions and be prepared. Try to be patient while waiting for phone updates and embryology information. We are taking care of your embryos, processing your gametes and those won’t wait for phone calls or accept apologies. We know you are anxiously waiting to hear updates and hear about your progress.
A good embryologist has excellent technical skills and is a very organized and detail oriented person. This field requires extensive documentation and protocol development. A person that has excellent hand eye coordination and an aptitude for paperwork is a great fit. Being a morning person is also beneficial as much of our work is complete before the sun even rises. We must be organized and work well under pressure.
Embryo grading:
The embryologist voice on the role of the IVF Lab in the treatment process, by Ashley Wong
I hope giving you an introduction to the infertility language and to embryology gives you comfort during a very stressful journey. The professionals in the embryology laboratory are often hard at work making sure everything is optimal before, during and after your cycle to help you build your family. We assist clinicians by providing them benchmark information, assessments and information that they consider when making treatment plans and protocols.
We are dedicated individuals who enjoy “babysitting” little cells and are impacted by your stories and journeys!
On a personal note, this job is not easy. We spend long hours in a small and often dark room without food or drink for hours. We stay until the work is done. Our hours are dependent on when patients get their trigger shot and our personal lives are completely dependent on our professional schedule. We often do not even meet or talk to the patients other than identification checks and embryo updates.
I chose this field because I am motivated to build families and give patients the love and joy my family brings me! Families grow in many different ways so the infertility journey a patient walks may be very different! Each patient comes to us with a different medical, ethical, religious and personal set of factors that they want considered.
We do our best to honour who they are as a person, couple (if applicable) and patient. I am very proud to look after their precious little embryos and take the responsibility very seriously.
I also view myself as their “first babysitter” in many ways. For example, we play music in the lab and often talk to gametes like they can hear us.
Patients that wear special socks, bring cookies/treats and teary “to be” dads always have an impact on me. I look for birth announcements and Holiday cards from the patients and feel a sense of great pride to see their families grow. I love meeting some of my children’s teammates and friends that I know I helped grow and watch them their first few days on this planet.
I have seen miracles that have strengthened my Faith and losses that have challenged it. I have celebrated with thousands and cried with some too.
I have participated in the care of thousands of patients but a few special cases will always stand out and have touched my heart. One case that really had an impact on me was a person that spent many hours, over many years, participating in my childrens’ lives and devoting much of themself to their development and talent. This person had a sibling that was affected by infertility and they sought out our clinic for treatment. I was so emotional over their care. I get teary today even writing about it. I wanted to give that couple and their family the same dedication, intensity of skill and devotion to their case that their sibling had given my family. I wanted so badly to give them the joy and love that I receive from watching my children develop! At their embryo transfer I disclosed that I knew their sibling and after I left the room became so emotional that I needed a minute to collect my composure before I performed the technical procedure of preparing their little embryos for transfer. They were successful in their treatment and I feel so happy to have been a part of that and to have repaid the spirit and energy given to me and my family!
Another patient story that had a different impact on me happened at a neighbourhood party many years ago where the host pulled me aside into a private room. I knew she was a parent of an adopted child because her child was similar in age to one of my children and I often saw her at school functions. In the private room she pulled out the embryo picture she was given at transfer. I remembered immediately that she had not been successful and was anxious about where the conversation might go. She quickly expressed gratitude and thanked me for my role in her journey and for the photo. When I expressed confusion about the gratitude for the photo she explained that the photo gave her something concrete to grieve. She said she needed to grieve the idea of carrying a pregnancy and a biological child.
After she had let go of that road in her journey, she could pursue a new path that included international adoption. This new path eventually led to her becoming a mother and having a family. That woman in turn has helped me weather many failures with the hope that if nothing else, we gave them closure that they tried everything they could before moving on to a different path or journey.
As you can see, the embryology laboratory team plays an important role in your treatment process. We are hard at work behind the scenes making sure the people, environment, equipment and supplies are all optimized for your success. You may not always see us, but we are always there keeping your embryos, stories, hopes, and dreams in our thoughts around the clock!
The “embryo Koala” photo

Resources:
- Revised minimum standards for practices offering assisted reproductive technologies, Fertility and Sterility Vol. 90, Suppl 3, November 2008
https://www.fertstert.org/article/S0015-0282(08)03722-9/pdf - Human embryo fragmentation in vitro andits implications for pregnancy and implantation, Fertility and Sterility Vol. 71, No. 5, May 1999,
https://www.fertstert.org/article/S0015-0282(99)00092-8/pdf - Standardization of grading embryo morphology, Fertility and Sterility Vol. 94, No. 3, August 2010,
https://www.fertstert.org/article/S0015-0282(10)00856-3/pdf - The simplified SART embryo scoring system is highly correlated to implantation and live birth in single blastocyst transfers, J Assist Reprod Genet. 2013 Apr;30(4):563-7,
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3644132/ - A Review of The Society for Assisted Reproductive Technology Embryo Grading System and Proposed Modification, Int J Fertil Steril. 2016 Jul-Sep;10(2):141-7
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4948064/
Table of Contents





Great view on embryology lab and importance of an embryologist in IVF treatment, as we – patients don’t really know what’s behind and how it’s managed in IVF laboratory.
Thank you! This should be read by everyone looking into IVF treatment and what’s going on in ivf laboratory. Thank you for emotional touch, it shows that you really care Ashley. It’s obvious that there is stron connections between embryo development and IVF success rates. You should read this article:
https://www.eggdonationfriends.com/ivf-success-rates-myths-figures-revealed/
From patient point of view it’s all about the doctor however as we can see above the embryologist role is very important maybe more important than a doctor… the IVF treatment is tricky as there are many things not uderstandable by patient so it’s great we have such articles and we need more regarding an IVF treatment and IVF procedures. And to be honest I’ve never seen an embryologists… and had IVF attemps without luck…